“I will be using a traditional birth attendant for my next delivery. The women there take care of you like you are their daughters”
These were the words of Theresa Usman, a new mother who asked that her real name not be used. Usman used one of the government-owned health facilities in Tamale, Ghana
Usman is not the only woman who dreads the treatment at some of the government-owned health facilities.
In Nigeria, Ijeoma Unachukwu and Peace Odiete were glad to have taken a prescient decision to register for a private ward service to dodge the mistreatment encountered during delivery, especially at some government-owned health facilities.
Peace went on to defend her decision saying “watching new mothers go to fetch water at the general hospital tap, I knew paying the premium price was the best decision for me”.
There has been growing evidence of poor health facilities and delivery in Ghana and Nigeria which significantly entails mistreatment, abuse and disrespect of women who especially have used government-owned health facilities
These abuses and disrespect frequently manifest in the form of ineffective and condescending communication, inadequate care and support, apathy during service delivery, and other actions and omissions that outrightly violates the right of women to quality mental and physical health service as enshrined in various national and international laws.
A systematic report conducted at a global scale in 2015, categorized the variant forms of mistreatment and abuse as either physical, sexual, or verbal abuse It also includes, stigma and discrimination; failure to meet professional standards of care; poor rapport between women and providers; health system conditions and constraints.
Both Nigeria and Ghana have a maternal mortality rate of 917 and 308 per 100,000 live births respectively. These fall short of the 2015 Development Goal Target, hence, efforts at improving safe motherhood in facility-based centers in both countries remain valid concerns.
Respectful Maternity Care
Respectful Maternity Care according to the Maternal Health Task Force MHTF is defined as an approach centered on the individual, based on principles of ethics and respect for human rights. It also promotes practices that recognize women’s preferences and the needs of both women and newborn. Promoting Respectful Maternity care (RMC) is being increasingly recognised as a critical element of improving the quality of maternity care across the globe. RMC is also described as a way to address issues like ‘disrespect and abuse’, ‘obstetric violence’ and ‘dehumanised care’
One of the organizations fronting the campaign to promote Respectful Maternity Care is the White Ribbon Alliance (WRA). In 2011, it launched a global campaign to produce and promote a legal framework for RMC entrenched in international human rights. A significant output of this campaign was the production of the Respectful Maternity Care Charter which was updated in 2018 to include the rights of newborns.
In 2013, one of the WRA milestones in Nigeria was the adoption of RMC as a federal policy by the Federal Ministry of Health’s (FMOH) National Health Council. The FMOH adopted a draft charter on the institutionalisation of RMC as a strategy to promote the reproductive rights of women in Nigeria. And this includes the right to quality maternity health services.
Other organizations inter alia are the International Federation of Gynaecology and Obstetrics (FIGO), the International Confederation of Midwives, the International Paediatrics Association and the World Health Organization.
In 2014, the World Health Organization released a statement for the prevention of disrespect and abuse during facility-based childbirth as a strong factor in promoting maternal health and wellbeing and consequently reducing maternal death.
In this statement endorsed by over 90 organizations, the WHO called for greater support and programs from governments to protect the rights of women to dignified, respectful healthcare through pregnancy and childbirth and improve the quality of maternal health care, with a strong focus on respectful care.
Contrary to the popular negative experiences of pregnancy and delivery reported in many health facilities in Nigeria and Ghana, mothers who have used the Bwari General hospital in Bwari, Nigeria and Korle Bu hospital in Accra, Ghana MC treatment have reported more positive experiences because both hospitals have adopted some form of Respectful Maternity Care
Bwari General Hospital, Nigeria
Adegoke Adebukola who had just had caesarean delivery at the time of our interview described her pleasant pregnancy experience at the hospital.
“Everything from my antenatal to post-delivery experience is good here. The nurses are so nice and they don’t get irritated by our numerous questions.
This hospital is good and I will recommend it for mothers either for normal delivery or caesarean delivery like I did.”
Abdullahi Tare is another mother who has used the Bwari general hospital and recounts her experience as a pleasant one.
Tare, who has been informed prior to delivery of having a major complication associated with her pregnancy, was very scared and was skeptical of her choice to use the government hospital.
However, the reassuring words from the health workers (both doctors and nurses) were what gave her the confidence to proceed with her delivery at the hospital.
“The encouragement I got from the nurses after delivery made me strong. You can see my baby and I are fine.”
This culture and distinct service delivery at the Bwari General Hospital was traced to a series of empowerment training for the health workers on Respectful Maternity Care (RMC) delivery, mostly provided by non-governmental organization and professional bodies
The training is designed for health workers who work closely with pregnant women and new mothers at the hospital in any of the obstetrics and gynaecology departments.
At the training, the health workers are trained on the provision of the Respectable Maternal Care Charter and their responsibilities in fulfilling these rights to the service users.
The Society of Gynecologist and Obstetrics in Nigeria (SOGON) is one of the bodies chairing on RMC implementation in Nigeria with support from the International Federation of Gynecology and Obstetrics (FIGO)
Between 2009 and 2013, FIGO introduced the FIGO LOGIC (Leadership in Obstetrics & Gynaecology for Impact and Change) funded by the Bill & Melinda Gates Foundation to strengthen the organizational capacity of eight national Member Associations (MAs) of Obstetricians and Gynaecologists in Africa and Asia, to improve policy and practice in maternal and newborn health.
One of the beneficiary association is the Society of Gynaecologist and Obstetrics in Nigeria (SOGON)
From the final LOGIC report, SOGON has been working to influence national policy on the development of Skilled Human Resources for maternal services making significant input into the development of the curriculum, training and manual for the deployment of midwives under the Midwifery Service Scheme (MSS).
Dr Nneka Onwu, the director of Community Health Service, at the National Primary Health Care Development Agency (NPHCDA) confirmed that the Society of Gynaecologist and Obstetrics in Nigeria (SOGON) and Federal Ministry of Health reviewed and updated training curriculum for maternal health workers to include Respectful Maternity care and according to global standards.
She further stated that there are ongoing efforts to institutionalise these trainings from the medical and health schools.
In Ghana, the head of the Safe Motherhood Program at the Ghana Health Service, Family Health Division where the RMC is domiciled, Dr Opoku Fofie says that the WHO has provided a mass technical support.
Equally, NGOs such as JICA have also supported training sessions to guide on integrating RMC as training components for all training modules offered to midwives.
Notwithstanding the positive feedbacks from mothers, the hospital has had its own share of challenges implementing the RMC
For example, the management had observed a gap in the number of capacity building training and number of maternal health workers available and had to design a quota system for selecting maternal health workers from different units i.e the labor room and post-natal room workers to attend training on RMC.
In addition, selected members for every training are mandated to step down the training upon completion.
This action thus helps to ensure that all maternal health workers are in the know of new information and general knowledge of RMC to improve service delivery to mothers and pregnant women alike
A deficit of human resources has equally posed a slamming impact in effectively implementing RMC.
One of the nurses who has been trained at the Bwari hospital complained that the huge gap in Patient to nurse ratio (usually 1 nurse to 10 patient) can be overburdening for the nurses who sometimes are not able to give adequate attention to the different mothers or pregnant women while on duty.
Along with this, managing the demands of family members and caregivers could further stretch the workload.
‘When we are trying our best to attend well to these women, we also have different demands from their family members to deal with. These demands are even sometimes not good for the woman’
An example of these demands could be family members adamantly bringing well-wishers to visit new mothers in general wards at unofficial visit hours.
These visits could bridge the privacy of other mothers in the ward.
Korle Bu Hospital, Accra Ghana
At the Korle Bu Hospital in Accra, Ghana, Respectful Maternity care is implemented under the ‘Positive Pregnancy Experience’ program with support from the Ghana Health Service
This program is designed with the premise that mothers who have used the facility at any stage between pregnancy and post-partum must report having a positive experience that cannot occur without respecting and meeting the woman at every point of her needs.
The program involves conscientization of women on their rights to RMC through a revised antenatal curriculum (called the positive pregnancy experience module); training of health workers; and an evaluative program that involves direct contact with service users.
During the evaluative program, mothers and pregnant women who have used the facilities are contacted directly to get their opinions and assessment of the service received at the hospital.
The guiding questions considered during this evaluation exercise are hinged on benchmarks such as cultural appropriateness, respect for privacy, treatment of complaints and general psychological needs of the women.
The auditing has especially helped to learn factors that impair women especially from using health-based facilities.
An endearing element of the positive pregnancy experience program at the Korle-Bu Teaching Hospital is the training of some health workers on sign language to ease communication and consequently better health delivery service to women living with hearing disabilities.
Dr Titus Beyou, Co-founder, Comprehensive Care Group and obstetrician at the Korle-Bu Teaching Hospital in Accra, Ghana describes RMC as an integral aspect of a holistic maternal health intervention care service.
Going further, he defined RMC as offering maternity services from the antenatal care, during delivery and even postpartum period that understands the psychosocial needs of the women for her to feel respected and cared for.
He explains that Respectful Maternity Care can be a strong factor for increasing the use of health-based facilities as against Traditional and Religious Based Birth delivery.
Rahinatu Ishaku who has worked for over the years as a nurse and midwife in the Northern region of Ghana informed that women at the rural communities are more prone to mistreatment for several factors such as illiteracy, ignorance or limited understanding of their rights, misperception of healthcare workers as authority figures, and some social-cultural factors.
Dr. Beyuo added that the continual mistreatment of women especially in rural areas is the reason why women in those areas opt for traditional birth attendants and religious houses where they are more prone to infections and cannot access basic complementary services like checking the weight of the child.
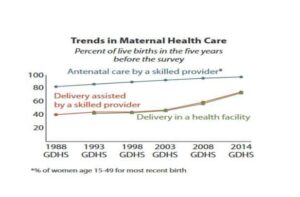 Data Source: 2014 Ghana Demographic and Health Survey
Data Source: 2014 Ghana Demographic and Health Survey
In addition, Respectful Maternity health can be used to abate obstetrics related complications as in the case of Vivian Okosi (who asked that her real name not be used) in Accra, Ghana.
Vivian Okosi suffered from Fistula some weeks after her delivery.
In her narration, she complained to the midwife at the hospital she used about not feeling good enough to be discharged after delivery but her complaint was disregarded by the midwife who claimed to have more professional experience to understand Vivian’s situation better and went ahead to discharge her.
It only took a few days later that Vivian developed full signs of fistula while at home, and was referred to the Korle-Bu Teaching Hospital for treatment.
Bar. Damilola Ogunsakin a gender activist’ says that when Respectful Maternity care is not availed to women, it isn’t just a mere case of mistreatment but a strong violation of human rights which are described in national and international laws ratified by the erring country
For example, article 14 (section 2b) and Article 16 of The Maputo protocol and African Charter on Human and Peoples’ Rights respectively place on the government the responsibility to provide the best attainable state of physical and mental health of its people.
Strengthening Implementation of RMC.
From his experience working as an obstetrician, Dr. Beyuo says he has observed the need for strengthening certain systemic and human factors, whilst ensuring that women are aware of these rights.
In his highlight, systematic factors would include a conscious effort within health-focused ministries, department and agencies targeted at continuously building the capacity of health workers on RMC and availing enabling facilities and structures to deliver a Respectable Maternal Care service which is enshrined in Article 6 of the Respectable Maternal Care Charter that requires that women have access to healthcare and the highest attainable level of care.
From the interviews with health providers, the shortage of health workers is another critical factor that must be considered to implement and promote RMC.
Globally, the WHO has estimated a need for 18 million more health workers by 2030 to reach the SDG targets on universal health coverage.
This estimate particularly requires nurses and midwives and is needed most in low- and middle-income countries. From a 2013 report by the United Nations International Children Emergency Funds (UNICEF), the largest global shortages of health workers were in Southeast Asia and Africa with a shortage of 6.9 million and 4.2 million respectively.
Having more health workers will impact quality care delivery as health providers are less burdened and can dedicate more time to adequately care for patients.
Dr Opoku Fofie opines that programs that increase the awareness of women to RMC is important to conscientise women, and increase their confidence to demand their rights.
He also went further to say that the “issues of RMC may not entirely be on knowledge of mothers but the conditions available for the woman”.
In view of the above, he purported that “there should be structures and facilities in place to empower women to insist on the sort of things they deserve” rather than subjecting them to adapt to what they can obtain regardless of the knowledge.
Empathetically, Dr. Chris Fofie asserts that an intersectoral collaboration and approach whereby RMC is addressed from the multi angle of gender, social education, economic issue, civic issue rather than just a health issue should be integrated.
In summary, he says”RMC is not something in a vacuum but something every woman deserves and we need to make sure every woman has it”
This story was produced with the support of a reporting grant from Maternal Figures and Code for Africa.

